Sleep apnea is a chronic medical condition that causes people to stop breathing during the night, specifically due to the blockage of the airway. This halts the flow of oxygen into the body and disrupts a person’s ability to have a restful and healthy sleep. To address sleep apnea, there are two main types of breathing support machines that help keep the airway open and deliver oxygen to the lungs at all times: BiPAP and CPAP. Patients and healthcare providers can select the right machine by understanding the difference between CPAP vs BiPAP.
Sleep apnea is a common and potentially dangerous condition in which you briefly stop breathing or have reduced breaths during your sleep. If left uncontrolled, it has some dangerous complications such as high blood pressure, heart ailment and even stroke.
CPAP is perhaps the most commonly used therapy among people suffering from sleep apnea. However, another kind of treatment known as bilevel positive airway pressure or BiPAP is usually prescribed to certain categories of patients.
This article aims to explain differences between CPAP vs BiPAP machines, the uses, pros, and cons of each equipment with respect to the different types of sleep apnea.
Understanding Sleep Apnea
It is necessary to understand that there are two types of sleep apnea before describing the workings of CPAP and BiPAP devices in detail. There are three primary forms:
- Obstructive Sleep Apnea (OSA): Has features of the most prevalence, is manifested by the complete or partial closure of the airway during the night.
- Central Sleep Apnea (CSA): This is a type of sleep-disorder that is characterized by the failure of the brain to transmit signals to the muscles responsible for breathing.
- Complex Sleep Apnea Syndrome: This involves, both obstructions and from the central nervous systems.
Both CPAP and BiPAP machines are mainly prescribed for OSA patients but can be employed in CSA and complex sleep apnea treatment as well.
CPAP: Continuous Positive Airway Pressure
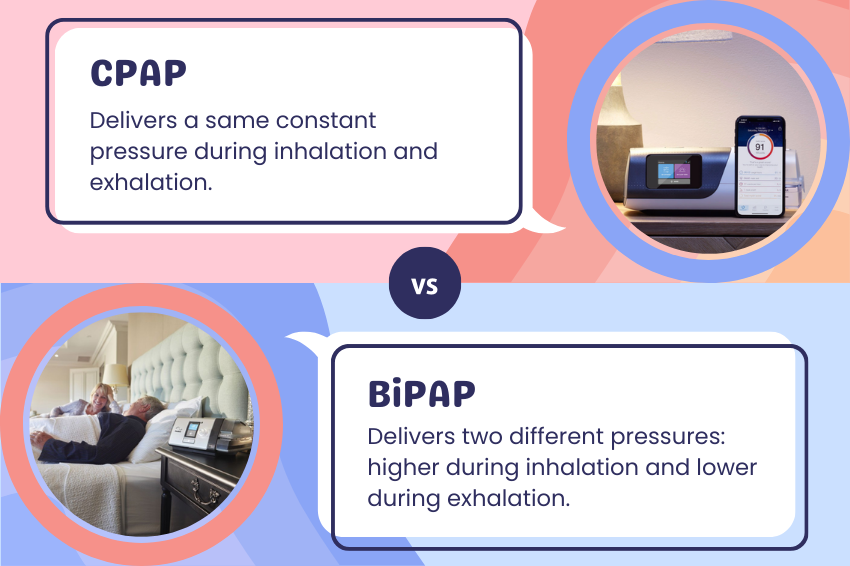
CPAP stands for Continuous Positive Airway Pressure. The device used to offer continuous and forceful blow to the air through a mask that acts as an air splint while sleeping. This continuous airflow makes sure that the airway does not collapse just like is the case with sleep apnea.
Benefits of CPAP
- Effectiveness: As stated earlier, CPAP is considered among the most effective therapies for moderate and severe OSA. As a result, it is helpful in decreasing or eradicating apnea occurrences and enhancing the quality of sleep.
- Ease of Use: The device is as basic as a wheelbarrow and has devised a simple approach of applying a continuous and constant pressure.
- Non-Pharmacological Treatment: CPAP is non-pharmacological and non-invasive method of treatment. Therefore, it is a better option as compared to surgery for the patients.
- Better Health Condition: CPAP use was also found to reduce the blood pressure, as well as promote daytime drowsiness and overall wellbeing among patients. It also minimizes the occurrence of cardiovascular complications that are associated with non-treated sleep disorders.
Drawbacks of CPAP
- Pressure: Some air pod wearers experience pressure coming from the use of air pods due to the unsuitable fit or existing claustrophobia conditions.
- Dryness: Due to the cool air that is produced by the airflow, the throat as well as the nasal passages may dry, resulting in congestion. This problem can however be addressed by the use of humidifiers.
- Noise: Despite the advanced technology in the current CPAP machines still produce some noise and the user may only find it intolerant.
- Compliance Problems: There are times that patients have difficulty in using the CPAP due to discomfort or inconvenience of usage.
BiPAP: Bilevel Positive Airway Pressure
BiPAP is an abbreviation for Bilevel Positive Airway Pressure. Not like CPAP that only has one pressure operating throughout the cycle, BiPAP is set to have two pressures; a high pressure during the inhaling process (IPAP) and low-pressure during exhaling (EPAP). This two-level pressure system can be useful to control the respiratory process and make it more natural and comfortable for those who have problems with the constant pressure in their lungs that is applied by CPAP.
Benefits of BiPAP
- Comfort: It is to some extent more comfortable for patients as they have to do less resistance in exhaling and the pressure surges during the composure of breathe contrast to the constant pressure of the CPAP.
- Versatility: BiPAP devices are customizable depending on the patient’s condition hence can be used by patients with different intensity of sleep apnea or other respiratory disorders.
- Relation to CSA and Complex Apnea: BiPAP may be more suitable for patients who suffer from CSA and complex apnea since the pressures are automatically adjustable to cater for the patent’s irregular breathing.
- Ease of Exhalation: Patient find it easier to breathe out while using bi-level vaporizer which reduce the feeling of breathlessness which is common with CPAP.
Drawbacks of BiPAP
- Cost: While the price of the BiPAP machines is distinguished to be slightly higher than that of the CPAP machines, the overall cost of using the BiPAP machines both initially and the subsequent expenses are also higher.
- Risk / Opportunity: There may be more applications of the adjustable settings, which may be complex in managing and could take more collective effort by the patient-end and the healthcare settings to achieve the right setting.
- Lack of Standardization: In comparison to CPAP, the effectiveness of BiPAP depends on the settings, and the particular state of the patient, which makes the general use of this type of therapy less standardized.
- Risk of Ineffective Treatment: BiPAP therapy may be ineffective in the treatment of OSA since the device may not offer adequate interventions to patients with severe epigenetic features of the disorder.
CPAP vs BiPAP Machines: Key Differences
Here’s a structured table comparing CPAP (Continuous Positive Airway Pressure) and BiPAP (Bilevel Positive Airway Pressure) machines, highlighting their key differences:
| Feature | CPAP | BiPAP |
|---|---|---|
| Full Name | Continuous Positive Airway Pressure | Bilevel Positive Airway Pressure |
| Pressure Delivery | Delivers a same, constant pressure during inhalation and exhalation. | Delivers two different pressures: higher during inhalation (IPAP) and lower during exhalation (EPAP). |
| Use Cases | Primarily for obstructive sleep apnea (OSA). | Used for OSA + complex conditions (e.g., central sleep apnea, COPD, neuromuscular disorders). |
| Comfort | Some users find exhaling against pressure uncomfortable. | Often more comfortable due to lower exhalation pressure. |
| Complexity | Simpler design, fewer settings. | More advanced, adjustable pressure settings. |
| Cost | Generally, less expensive. | Typically, more expensive due to advanced features. |
| Pressure Relief | May offer “ramp” features but no pressure relief during exhalation. | Built-in pressure relief (like “Bi-Flex” or “A-Flex”). |
| Typical Patients | Mild to moderate OSA patients. | Severe OSA, central sleep apnea, or patients with respiratory insufficiency. |
| Oxygen Integration | Can be paired with oxygen, but less common. | Often used with supplemental oxygen. |
CPAP vs BiPAP: How to Choose the Right Machine
Factors to Consider
- Type of Sleep Apnea: The CPAP therapy is commonly prescribed to patients with obstructive sleep apnea whereas BiPAP therapy can be more appropriate in the cases of central or complex sleep apnea.
- Severity of Apnea: The patients with severe OSA normally benefit from CPAP more than BiPAP is used in cases moderate to severe OSA where the patient cannot use the CPAP because of this or that other condition.
- Tolerance: Since there are always unconscious moments during the daytime, the patients may not endure the CPAP pressure levels and instead, comfort would necessitate BiPAP with its versatile pressure range.
- Medical Conditions: BiPAP is especially beneficial for patients with such other illnesses as Chronic Obstructive Pulmonary disease (COPD) or heart failure.
- Cost and Insurance: Another consideration is the cost difference in the two machines, mainly the CPAP and BiPAP machines and the insurance coverage that is available in relation to these two machines.
Consulting Healthcare Providers
For a patient, there is need to seek the support of his/her doctor in order to know the suitable treatment to undergo. A dentist or a professional can have the patient undergo a sleep study and be in a position to determine the kind of sleep apnea the patient is experiencing and the extent of it so that the doctor is in a position to recommend the best treatment plan.
Trial and Adjustment Period
Every one of the two therapies needs a little adjustment to the therapy modality by the users. The patients should preferred mask, pressure, and the configuration of the humidifier may vary depending on needs of the patient. They should attend follow up visits in order to determine if the treatment is working and to have a change if it is necessary.
Conclusion
Both the CPAP and BiPAP machines provide very useful treatment for sleep apnea with differences and similarities in their usage. Obstructive sleep apnea is mainly treated with the use of CPAP primarily because of its ease of use and efficiency. Nevertheless, BiPAP may be more suitable for patients who cannot use CPAP or have central or complex sleep apnea, or other pulmonary diseases.
It is also important to note that the selection between CPAP vs BiPAP should be made according to the patient’s requirements and tolerance levels as well as recommendation by medical practitioners. Hence, proper patient management will help patients have improved sleep quality, better health status, and quality living.