Menopause is a normal biological occurrence. When a woman experiences it, their menstrual cycle comes to an end. However, the mental and physical side effects of menopause, such as hot flashes, might impair your emotional well-being, cause sleep disturbances, or sap your energy.
Hormone therapy is one of the many efficient treatments available, along with lifestyle modifications. Although it is a common experience for women, each woman’s path through it will be different, with symptoms and experiences ranging greatly.
When a person has missed 12 consecutive months of their menstrual cycle, they enter the menopause. Marking the end of your reproductive years, it is a normal aspect of ageing. Continue reading about the menopause symptoms, causes, and treatment:
What is menopause?

When you cease getting monthly periods, the stage in life is known as menopause This marks the end of your reproductive stage and occurs when your ovaries spontaneously stop generating eggs. Most women experience this between the ages of 45 and 60. It usually sets at around age 51. It is the state in which a woman reaches the 12-month mark without menstruation.
There are various medical conditions that can lead to early menopause in some people, including primary ovarian insufficiency. In addition, it may occur after ovarian or uterine cancer treatment or after surgery.
Every woman has a unique menopausal experience. Some people simply endure little discomfort, while others have more serious side effects. Although they can persist for years, symptoms are often transient.
What are the three stages of menopause?
The menstrual cycle permanently terminating on its own without the need for medical intervention is known as natural menopause. There are three phases to the progressive process:
- Transitional menopause or perimenopause: Your ovaries progressively start to generate less estrogen eight to ten years before menopause, which is when perimenopause starts. Usually, it begins in your 40s. Menopause, which occurs when your ovaries cease producing eggs, follows perimenopause. The final year or two of perimenopause sees an acceleration of the estrogen decline. Many people may be experiencing menopause symptoms at this point. However, you can still become pregnant during this time and still have menstrual cycles.
- Menopause: The menstrual cycles end when an individual reaches menopause. Your ovaries have finished producing most of their estrogen and are no longer releasing eggs. When you have missed your monthly cycle for 12 months in a row, a medical professional will diagnose you with menopause.
- Post menopause: Post menopause is the period following a year without menstruation. Menopausal symptoms, such as hot flashes, may improve during this phase. Nonetheless, a decade or more following the menopause transition, some women still have menopausal symptoms. People in the postmenopausal phase are more susceptible to several health issues, including osteoporosis and heart disease, due to a decreased level of estrogen in their bodies.
Why does menopause occur?
Estrogen, progesterone, and other hormones change as you age, causing a normal process known as menopause. The decrease in active ovarian follicles is connected to these alterations. Menstruation and fertility are made possible by these structures, which also create and release eggs from the ovarian wall.
It can sometimes come on early as a result of pelvic injuries, radiation therapy, chemotherapy, surgery, or other conditions that impair the reproductive system.
Everyone born with a feminine gender assignment will eventually go through menopause. It may occur during or following hormone therapy or surgery for gender transformation. Regardless of the gender or sex assigned at birth, shifts in specific hormone levels can cause menopausal symptoms.
What causes menopause?
-
Natural menopause
It is a natural process that starts when a woman’s ovaries run out of eggs to release. Oestrogen levels fall throughout menopause, causing symptoms to manifest. Hormone levels can fluctuate as the body changes leading up to the natural menopause.
-
Menopause early
Medical therapies like chemotherapy and radiation therapy for cancer that cause the ovaries to cease functioning can cause early menopause.
-
Vaginal dryness and discomfort
Dryness, itching, and pain during sexual activity might result from changes in the vaginal tissues brought on by the menopausal drop in estrogen levels. Sexual health and general quality of life are affected by this for women.
-
Emotional fluctuations and mood swings
Emotions and mood can be affected by changes in hormone levels. Mood swings, impatience, and feelings of anxiety or despair are common throughout menopause for women. For mental health, comprehending these shifts and getting help when needed can be essential.
-
Gaining weight and alterations in body composition
Changes in body composition and metabolism can be attributed to hormonal fluctuations. During this stage, many women may observe a shift in the distribution of body fat and an increase in abdominal fat.
-
Bone density loss
Osteoporosis risk can increase due to a decrease in bone density brought on by a loss in estrogen levels. One of the most important aspects of menopause therapy is bone health.
-
Sleep-related issues
Hormone fluctuations have the potential to interfere with sleep cycles and cause insomnia or restless nights. Sleep disruptions can exacerbate fatigue and general discomfort when paired with other symptoms.
-
Libido fluctuations
Hormone fluctuations can affect arousal and sexual desire. While some women may not notice any noticeable changes, others may report a decline in libido throughout menopause.
-
Gaining weight and alterations in body composition
Changes in body composition and metabolism can be attributed to hormonal fluctuations. During this stage, many women may observe a shift in the distribution of body fat and an increase in abdominal fat.
-
Loss of bone density
Osteoporosis risk can increase due to a decrease in bone density brought on by a loss in estrogen levels. One of the most important aspects of therapy is bone health.
How is early menopause treated?
Treatment for early or premature menopause may vary depending on the causes of the earlier-than-usual onset of menopause. Due to the health risks of early menopause, providers recommend hormone replacement therapy unless there is clear evidence that it is unsafe.
HRT replaces some of the hormones that are absent from your body. By doing this, you reduce your risk of experiencing the signs and adverse effects of early or premature menopause and related health problems. Providers typically advise HRT up until the patient reaches 51.
You must discuss the advantages and disadvantages of hormone therapy with your healthcare provider. Consult a fertility specialist to explore your alternatives if your infertility stems from early or premature menopause. They can help you fulfill your goal of becoming a parent.
Symptoms
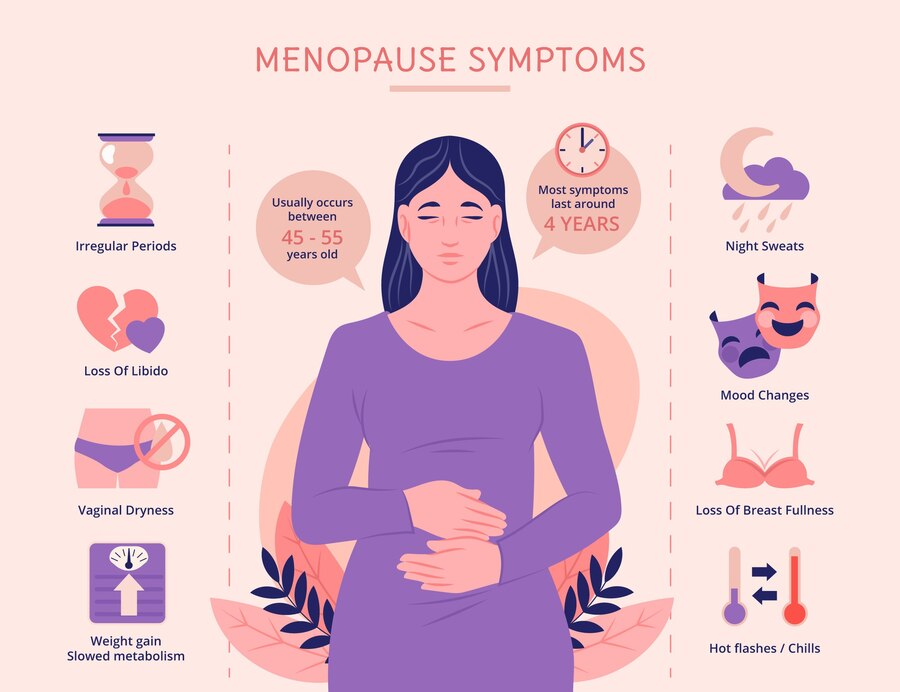
You may experience irregular periods, dry vagina, hot flashes, chills, night sweats, sleep issues, mood swings, weight gain, reduced metabolism, thinning hair, dry skin, and loss of breast fullness in the months or years before menopause.
Each woman may experience different signs and symptoms, including variations in menstruation. Before your periods cease, you may notice some abnormality in them.
Period skipping is normal during the perimenopause. Menstrual cycles frequently skip a month before returning, or they may skip several months before beginning again for a few months. Additionally, periods typically occur on shorter cycles, meaning they are closer together. Pregnancy is possible even with irregular periods. Consider taking a pregnancy test if you have missed a period but are unsure if the menopausal transition has begun.
When to see a doctor
Continue seeing your doctor regularly for any medical problems and preventive care. Maintain scheduling of these consultations both during and after menopause.
As you age, prescribed health screening tests, including mammograms, colonoscopies, and triglyceride screenings, may be part of preventive healthcare. In addition, if your medical history suggests it, your doctor may offer additional tests and examinations, such as a thyroid test and a pelvic and breast check.
If you experience vaginal bleeding after menopause, you should always consult a doctor.
Treatment options for menopause
-
Hormone replacement therapy
HRT is the use of estrogen to treat menopausal symptoms, frequently in conjunction with progesterone. It can be applied topically as creams, tablets, patches, or vaginal rings, among other forms.
-
Moisturizers and lubricants for the vagina
Over-the-counter vaginal lubricants and moisturizers can be used to treat vaginal dryness and pain. These goods alleviate discomfort and improve it during intercourse.
-
Non-hormonal medications
Certain menopausal symptoms can be managed with the use of several non-hormonal drugs. Selected serotonin reuptake inhibitors are antidepressants that are frequently administered to treat hot flashes and mood swings. Originally developed as an antiepileptic medication, gabapentin has also demonstrated efficacy in lowering hot flashes.
-
Techniques to promote bone health
Maintaining strong and healthy bones is crucial to preventing the loss of bone density. Weight-bearing activities and sufficient calcium and vitamin D consumption support healthy bones and lower the risk of osteoporosis.
-
Lifestyle modifications
Living a healthy lifestyle has a big impact on how menopause feels. Frequent exercise enhances mood, aids weight management, and promotes general well-being. Bone health is enhanced by a balanced diet rich in calcium and vitamin D. Techniques like yoga or meditation to manage stress can help reduce emotional problems.
Summing it up
The above details are about menopause symptoms, causes, and treatment. A woman’s menopause is a normal and unavoidable stage of life. Understanding the definition, causes, symptoms, and available therapies will equip women to confidently manage this transforming journey, even though the obstacles and symptoms may differ. They are maintaining open lines of communication with medical experts and taking a proactive stance on health.